Researchers develop new 3D technique: Innovation to treat Diabetic Foot Ulcer
Queen's University Belfast has come out with a new bandage treatment, known as a scaffold, to treat diabetic foot ulcers & also cost-effective while improving patient outcomes
- 3D printing method was first demonstrated in the 1980s and has grown rapidly in recent years due to technological developments
- The new research demonstrates outcomes with significant implications for patient quality of life, as well as decreasing the costs and clinical burden in treating DFU
- The annual incidence of diabetic foot ulcer worldwide is between 9.1 to 26.1 million, according to BLK Max Sr Physician and Sr director
Trending Photos
) Representational Image
Representational Image New Delhi: Diabetes, a lifelong condition that causes a person's blood sugar level to become too high, is among the top ten causes of deaths worldwide. Diabetic foot ulcer (DFU), is a serious complication of diabetes, affecting approximately 25% of diabetic patients. When identified, over 50 per cent are already infected and over 70 per cent of cases result in lower limb amputation. Queen's University Belfast has come out with a new bandage treatment, known as a scaffold, to treat diabetic foot ulcers & also cost-effective while improving patient outcomes.
The 3D printing method was first demonstrated in the 1980s, and since then, the field of 3D printing (3DP) and bioprinting has grown rapidly in recent years due to technological developments and a greater understanding of the capabilities using these technologies, particularly in the development of scaffolds for tissue engineering applications. In the fabrication of 3D (bio) printed scaffolds, the user is firstly required to design a scaffold using computer-aided design (CAD).
Specialist software can then be used to slice the design prior to printing, providing a set of printing instructions for the printer; each 3DP manufacturer provides the software. A wide range of advantages is offered by 3DP, including the capability to rapidly produce elaborate (scaffold) designs of various sizes at low cost. Moreover, 3D-bioprinted scaffolds have shown the ability to achieve high cell loading and maintain high levels of cell viability while also providing structural support to the wound.
The treatment strategy required for the effective healing of diabetic foot ulcer (DFU) is a complex process that is requiring several combined therapeutic approaches. As a result, there is a significant clinical and economic burden associated in treating DFU. Furthermore, these treatments are often unsuccessful, commonly resulting in lower-limb amputation.
Graphical abstract
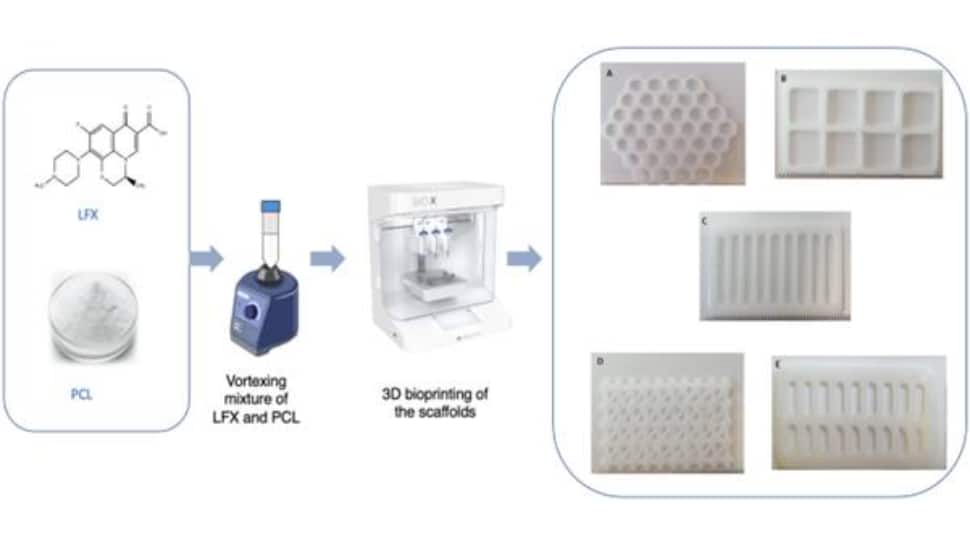
This new research demonstrates outcomes with significant implications for patient quality of life, as well as decreasing the costs and clinical burden in treating DFU. Recent research has focused on drug-loaded scaffolds to treat DFU. The scaffold structure is a novel carrier for cell and drug delivery that enhances wound healing.
Springler Link Research
The research, published in Springer Link, was presented by Professor Lamprou at the Controlled Release Society (CRS) Workshop Italy.
Professor Dimitrios Lamprou, a Professor of Biofabrication and Advanced Manufacturing at Queen's School of Pharmacy and corresponding author, explains: "These scaffolds are like windows that enable doctors to monitor the healing constantly. This avoids needing to remove them constantly, which can provoke infection and delay the healing process.
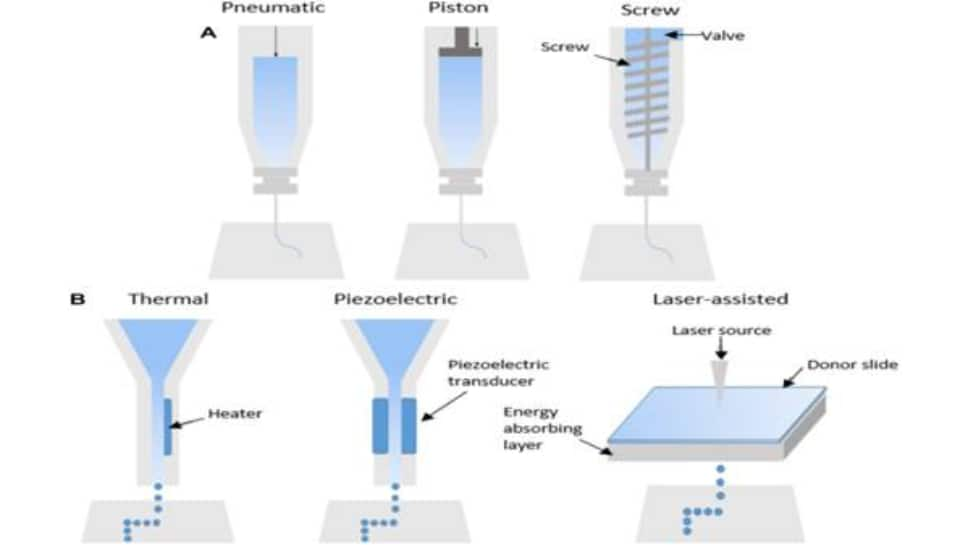
Schematics showing (a) extrusion-based, (b) inkjet-based, and (c) laser-assisted bioprinting technologies
"The 'frame' has an antibiotic that helps to 'kill' the bacteria infection, and the 'glass' that can be prepared by collagen/sodium alginate can contain a growth factor to encourage cell growth. The scaffold has two molecular layers that both play an important role in healing the wound."
What experts say
According to expert Ashok Jhingan , Sr Phycisian & Sr director BLK Max, "the annual incidence of diabetic foot ulcer worldwide is between 9.1 to 26.1 million. Around 15 to 25% of patients with diabetes mellitus will develop a diabetic foot ulcer during their lifetime.
The majority of patients with diabetes who develop foot ulcers are male (more than two-thirds). Furthermore, most of them are between 40 and 70 years of age. Older patients face significantly more complications than younger ones.
Diabetic peripheral neuropathy is a precipitating factor in almost 90% of diabetic foot ulcers. Chronically high glucose (blood sugar) levels damage nerves, including the sensory, motor and autonomic nerves. Diabetic neuropathy also damages the immune system and impairs the body's ability to fight infection.
Infection is a frequent (40%-80%) and costly complication of these ulcers and represents a major cause of morbidity and mortality. It is estimated to be the most common cause of diabetes-related admission to hospital and remains one of the major pathways to lower-limb amputation.
Dr. Jhingan also states that the most common risk factors for ulcer formation include diabetic neuropathy, structural foot deformity and peripheral arterial occlusive disease.New bandage therapy, called scaffold, has been created to treat diabetic foot ulcers (DFT) that is less expensive while also providing better patient outcomes by researchers at Queen's University Belfast.
The scaffolds, which are created by 3D bioprinting, gradually release antibiotics over a period of four weeks to cure the wound. The Journal of Drug Delivery and Translational Research published the study.Diabetes is counted among the top 10 causes of death worldwide. It is a lifelong condition that raises a person's blood sugar levels.
A devastating consequence of diabetes, diabetic foot ulcers (DFU) affect about 25 per cent of diabetic patients. More than 50 per cent of cases when discovered are already infected, and more than 70 per cent of them require lower limb amputation.In order to effectively treat DFU, a complex treatment plan comprising several combined therapeutic approaches is required. As a result, treating DFU entails a severe clinical and financial burden. Amputation of the lower limbs is frequently required since these treatments are often unsuccessful.
This new study shows results that have significantly affected patients' quality of life and reduced the expense and clinical burden of treating DFU. Drug-loaded scaffolds have been the subject of recent research to cure DFU. The scaffold structure is a novel carrier for cells and medications that improves wound healing.
|
Bioprinting technology |
Advantages | Disadvantages |
| Inkjet-based bioprinting |
|
|
| Extrusion-based bioprinting |
|
|
| Laser-assisted bioprinting |
|
|
How to prevent foot ulcers?
Dr. Ashok Jhingan states - wearing clean, dry socks that don't have tight elastic bands, which may restrict blood flow to the foot. Doctors advise people with diabetes to avoid walking barefoot and wearing sandals, which expose your feet to splinters, concrete, or sand, which may scrape or irritate the foot.
Keeping your diabetic wounds clean and free from infection is order number one. Some simple diabetic wound healing products include regular antibiotic ointments like Polysporin or Neosporin.
Stay informed on all the latest news, real-time breaking news updates, and follow all the important headlines in india news and world News on Zee News.
Live Tv







)
)
)
)
)
)
)
)
)
)

